By the numbers: A rising death rate.
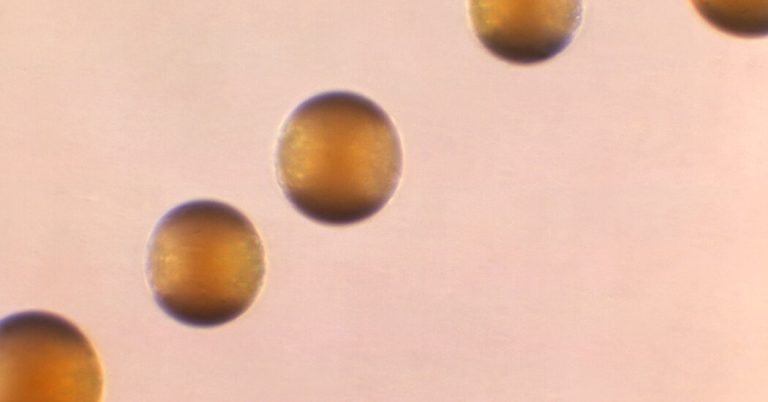
The disease is caused by infection with a bacterium called Neisseria meningitidis. Last year, 422 cases of invasive meningococcal disease were reported in the United States, the highest number since 2014, according to the Centers for Disease Control and Prevention.
However, as of Monday, 143 cases have been reported to the CDC so far this year, 62 more than the number of cases reported last year at the same time.
The disease is extremely dangerous. Even with appropriate treatment, 10 to 15 percent of patients who develop meningococcal disease will die. Many recent cases have been caused by an unusual strain of N. meningitidis called ST-1466. This strain caused 17 deaths among 94 patients whose results are known, a mortality rate of 18%.
Survivors of meningococcal disease may have long-term disability, deafness, amputations, or brain damage.
The Mystery: What Causes Breakouts?
The majority of people affected by the recent outbreaks were black and adults between the ages of 30 and 60.
Others who are susceptible to the infection include people living with HIV, who make up 15 percent of patients. people who have had their spleen removed. people with sickle cell disease. and patients with certain rare immune disorders.
A meningitis vaccine that protects against four of the six types of N. meningitidis — including the Y group, which includes ST-1466 — is recommended for teenagers as well as people with medical conditions such as HIV. Most older adults have not received the vaccine.
In Virginia, which has had 35 cases of meningococcal disease and six deaths since the summer of 2022, public health officials have found no epidemiological link to explain the outbreak, said Dr. Lori Forlano, a state epidemiologist.
“We’re always trying to find that golden ticket of common risk factors,” Dr. Forlano said. “Were they all together at a party or a family function? Were they all at a particular facility? Are there social networks that share? That just doesn’t happen here.”
The disease is not spread through casual contact, but through activities involving exposure to saliva or respiratory or throat secretions – for example kissing or sharing food and drink or cigarettes.
A ticking clock: Treatment must be done quickly.
The infection can cause meningitis, an inflammation of the membranes covering the brain and spinal cord. Typical symptoms include fever, headaches, neck stiffness, vomiting, sensitivity to light, and altered mental status.
The bacteria can also invade the bloodstream, a complication called sepsis, which appears to be the most common consequence with current cases of serogroup Y. Symptoms include fever and chills, fatigue, vomiting, cold hands and feet, severe pains, diarrhea, rapid breathing and, in later stages, a dark purple rash.
Symptoms can rapidly intensify and become life-threatening within hours. Antibiotics should be given immediately.
“With meningococcal disease, people’s thoughts go to meningitis, which is a very scary condition,” Dr. Forlano said. “But the point we’re trying to make in the clinical community is that these cases present differently than what we’re used to seeing. Well, hey, think about it.’
Despite the risk, however, he stressed that the disease remains rare. “The threat to the general public is low,” he said.